Can Schizophrenia be Caused by Trauma? A Comprehensive Guide
Schizophrenia is a complex mental health disorder characterized by disturbances in thinking, perception, emotions, and behavior. Traditionally viewed as primarily a neurodevelopmental condition with genetic and environmental factors playing significant roles, there has been increasing interest and research into the potential role of trauma in its onset or exacerbation.
While schizophrenia has long been understood through a neurobiological lens, recent studies have explored how traumatic experiences might influence its development or severity.
However, the exact relationship between trauma and schizophrenia remains a subject of ongoing investigation, with researchers aiming to elucidate whether trauma can act as a trigger or a contributing factor in the manifestation of symptoms.
Individuals with schizophrenia have a higher risk of premature death compared to the general population, often due to co-occurring health issues, including higher rates of suicide, substance use disorders, and physical health problems such as cardiovascular disease.
The Link Between Trauma and Schizophrenia
The potential link between schizophrenia and trauma has garnered significant attention in psychiatric research. While schizophrenia is widely recognized as a neurodevelopmental disorder influenced by genetic predispositions and brain chemistry, emerging studies suggest that traumatic experiences could play a role in its onset or exacerbation.
Researchers are investigating how severe or prolonged trauma, such as childhood abuse, neglect, or exposure to violence, may contribute to the development of schizophrenia in vulnerable individuals.
It is important to note that not everyone who experiences trauma develops schizophrenia, highlighting the complex interplay of genetic, environmental, and individual factors in mental health outcomes.
Can Head Injury and Brain Trauma Cause Schizophrenia?
Head injuries and brain trauma have been studied extensively to understand their potential links to schizophrenia. While the majority of schizophrenia cases are associated with genetic and neurodevelopmental factors, there is evidence suggesting that severe head injuries or traumatic brain injuries (TBIs) could increase the risk of developing schizophrenia in some individuals.
Traumatic brain injuries, especially those resulting in significant structural or functional brain changes, may disrupt neural circuits and neurotransmitter systems implicated in schizophrenia. These disruptions can potentially trigger or exacerbate symptoms of the disorder.
However, the relationship between head injuries and schizophrenia is complex and not fully understood, as not all individuals who experience head trauma develop schizophrenia.
Ongoing research aims to clarify the specific mechanisms through which head injuries might contribute to the onset or progression of schizophrenia, highlighting the importance of comprehensive neurological assessments and tailored interventions for individuals at risk.
What is Trauma-Induced Schizophrenia?
Trauma-induced schizophrenia refers to a subset of cases where traumatic experiences, such as severe physical or emotional trauma, are believed to contribute significantly to the development or exacerbation of schizophrenia symptoms.
While the exact mechanisms are not fully elucidated, researchers theorize that traumatic events may alter brain function, disrupt neural pathways, and affect neurotransmitter systems involved in regulating mood, perception, and cognition.
This alteration could potentially increase susceptibility to psychotic symptoms characteristic of schizophrenia, such as hallucinations, delusions, and disorganized thinking. It’s important to note that trauma-induced schizophrenia is considered a complex interplay of genetic vulnerability and environmental triggers rather than trauma being the sole cause.
Understanding this phenomenon requires careful consideration of individual differences in response to trauma and the broader context of psychiatric and neurobiological factors influencing mental health outcomes.
Can PTSD Turn into Schizophrenia?
Post-traumatic stress disorder (PTSD) and schizophrenia are distinct psychiatric disorders, each with its own set of symptoms and diagnostic criteria. While PTSD can involve symptoms such as intrusive memories, hypervigilance, and emotional numbness following exposure to a traumatic event, it is not known to transition into schizophrenia directly.
However, there is evidence suggesting that individuals with PTSD may be at a higher risk of developing schizophrenia later in life, particularly if they experience ongoing severe stressors or if there is a pre-existing vulnerability to psychotic disorders.
The relationship between PTSD and schizophrenia is complex and multifaceted, often involving overlapping symptoms such as hallucinations or emotional dysregulation.
PTSD VS Schizophrenia
| Feature | PTSD | Schizophrenia |
| Primary Symptoms | Intrusive memories, hypervigilance, avoidance | Hallucinations, delusions, disorganized thinking |
| Trigger | Traumatic event (e.g., combat, assault) | Genetic predisposition, environmental stressors |
| Onset | Typically follows trauma | Adolescence to early adulthood |
| Neurobiology | Hyperarousal, amygdala involvement | Dopamine dysregulation, enlarged ventricles |
| Treatment | Cognitive-behavioral therapy, exposure therapy | Antipsychotic medication, psychosocial support |
| Prognosis | Symptoms may improve with treatment | Chronic condition, variable outcomes |
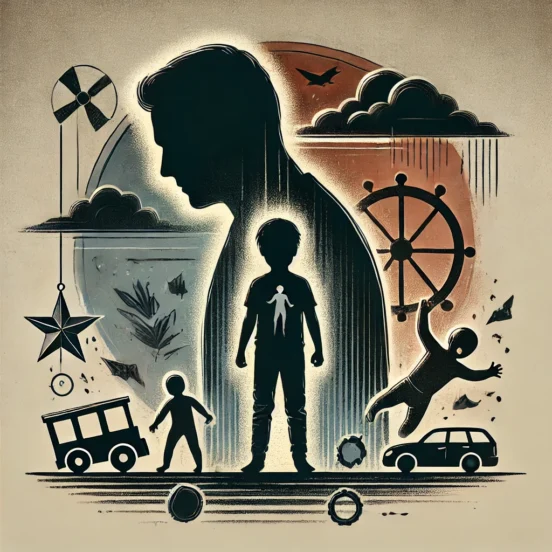
Childhood Trauma and Schizophrenia
The role of childhood trauma in the development of schizophrenia has been a subject of considerable research and debate. While schizophrenia is primarily understood as a neurodevelopmental disorder influenced by genetic and environmental factors, there is growing evidence suggesting that early-life adversities, such as abuse, neglect, or unstable family environments, may contribute to an increased risk of developing schizophrenia later in life.
The question of “Does childhood trauma cause schizophrenia?” remains complex and multifaceted. Studies indicate that traumatic experiences during critical periods of brain development may alter neural circuits and stress-response systems, potentially increasing vulnerability to psychosis.
However, it’s important to note that not all individuals who experience childhood trauma develop schizophrenia, highlighting the importance of genetic predispositions and other environmental factors in the onset of the disorder.
Can Adults Develop Schizophrenia from Trauma?
Schizophrenia typically manifests in late adolescence or early adulthood; there is evidence to suggest that traumatic events experienced in adulthood, such as severe stress, physical or emotional abuse, or significant life changes, might trigger or exacerbate psychotic symptoms in individuals already predisposed to the disorder.
This relationship, however, is not straightforward. Trauma in adulthood alone is unlikely to cause schizophrenia; instead, it may act as a catalyst in those with underlying vulnerabilities, including genetic factors and early-life experiences.
The interaction between trauma and schizophrenia underscores the importance of a comprehensive approach to mental health that considers both past and present experiences, as well as the individual’s broader psychological and biological context.
Effective treatment and support can help manage symptoms and improve outcomes for those affected.
Schizophrenia Triggers
Schizophrenia is a multifaceted mental health disorder with a variety of potential triggers. Understanding these triggers is crucial for early intervention and management of the condition. Common triggers include genetic predisposition, as schizophrenia often runs in families, and environmental factors, such as prenatal exposure to infections or malnutrition.
Genetic Factors
Genetic predisposition is one of the most significant risk factors for schizophrenia. Individuals with a family history of schizophrenia are at a higher risk of developing the disorder. Research has identified several genes associated with an increased risk of schizophrenia, suggesting a hereditary component.
However, genetics alone do not determine the onset of schizophrenia, indicating that environmental factors also play a critical role in conjunction with genetic vulnerabilities.
Environmental Stressors
Environmental stressors, such as exposure to traumatic events, significant life changes, or chronic stress, can act as triggers for schizophrenia. These stressors may disrupt brain function and contribute to the onset or exacerbation of symptoms in individuals with a genetic predisposition.
Understanding the role of environmental stressors in schizophrenia is essential for developing effective prevention and intervention strategies, particularly for those at high risk.
Substance Abuse
Substance abuse, particularly the use of psychoactive drugs like cannabis, amphetamines, or hallucinogens, has been linked to the development and worsening of schizophrenia symptoms.
These substances can alter brain chemistry and potentially trigger psychotic episodes in vulnerable individuals. Addressing substance abuse is a critical component of managing schizophrenia and preventing symptom exacerbation.
Neurobiological Factors
Neurobiological factors, including imbalances in neurotransmitters such as dopamine and glutamate and structural abnormalities in the brain, are crucial in the development of schizophrenia. These factors can influence the onset and progression of the disorder, affecting cognitive functions, emotional regulation, and perception.
Ongoing research into neurobiological factors aims to uncover more about the underlying mechanisms of schizophrenia, which could lead to improved treatments and therapeutic approaches.
Myths about Schizophrenia and Trauma
There are numerous myths surrounding the relationship between schizophrenia and trauma, which can lead to misunderstandings and stigma. One common misconception is that trauma alone can directly cause schizophrenia when, in fact, the development of schizophrenia is influenced by a complex interplay of genetic, environmental, and neurobiological factors.
Myth: Trauma Alone Causes Schizophrenia
Reality: Schizophrenia arises from a combination of genetic predisposition, environmental influences, and neurobiological factors. Trauma may increase the risk but is not the sole cause.
Myth: People with Schizophrenia are Violent
Reality: Most individuals with schizophrenia are not violent and are more likely to be victims of violence than perpetrators.
Myth: Schizophrenia is a Split Personality Disorder
Reality: Schizophrenia is often confused with dissociative identity disorder (multiple personality disorder), but it is a distinct condition characterized by symptoms such as hallucinations and delusions.
Myth: Schizophrenia Cannot be Treated
Reality: While schizophrenia is a chronic condition, various treatments, including medication and therapy, can help manage symptoms and improve quality of life.
Myth: Only Genetic Factors Matter
Reality: Although genetics play a significant role, environmental factors like prenatal conditions, substance abuse, and trauma also contribute to the risk of developing schizophrenia.
Myth: Schizophrenia Develops Suddenly Without Warning
Reality: Schizophrenia typically develops gradually, with early warning signs often appearing during adolescence or early adulthood, including social withdrawal, unusual thoughts, and changes in behavior.
Myth: Schizophrenia Means Constant Psychosis
Reality: People with schizophrenia experience periods of relative stability and may not always exhibit psychotic symptoms. With proper treatment, many individuals can manage their symptoms effectively and lead fulfilling lives.
Myth: People with Schizophrenia Can’t Hold Jobs or Function in Society
Reality: Many individuals with schizophrenia can work and live independently with the right support and treatment. Occupational therapy, vocational training, and community support can help them achieve and maintain employment and social integration.
How to Prevent Schizophrenia?
Preventing schizophrenia is a challenging task due to its complex and multifactorial nature. While it is not possible to entirely prevent the disorder, early intervention and risk reduction strategies can significantly mitigate its impact.
Key prevention methods include maintaining a healthy lifestyle, managing stress, and avoiding substance abuse, particularly psychoactive drugs that can trigger psychotic episodes. Prenatal care is also crucial, as ensuring a healthy pregnancy can reduce the risk of neurodevelopmental issues.
Additionally, early identification of symptoms and timely intervention, such as counseling or therapy, can help manage potential risk factors and prevent the progression of the disorder.
Supportive environments, strong social connections, and access to mental health resources play vital roles in reducing the likelihood of developing schizophrenia or lessening its severity.
Bottom Line
The question “Can trauma cause schizophrenia?” reveals a complex interplay between genetic, environmental, and neurobiological factors. While trauma, especially in childhood, may increase the risk of developing schizophrenia in individuals with a genetic predisposition, it is not considered a sole cause.
Understanding this intricate relationship helps in tailoring prevention and intervention strategies, emphasizing the importance of early detection, supportive environments, and comprehensive mental health care.
FAQs
Question 1: Can schizophrenia resolve on its own?
Ans: Schizophrenia typically does not resolve on its own. It is a chronic condition that requires ongoing treatment and support to manage symptoms effectively.
Question 2: How long does schizophrenia last?
Ans: Schizophrenia is a lifelong condition. While symptoms can be managed with proper treatment, the disorder itself persists throughout a person’s life.
Question 3: Is schizophrenia 100% curable?
Ans: Schizophrenia is not 100% curable. However, with appropriate treatment, individuals can manage symptoms, achieve stability, and lead fulfilling lives.
References
Title: What is the link between trauma and schizophrenia?
Link: https://www.medicalnewstoday.com/articles/trauma-and-schizophrenia
Written & Published By: Medical NEWS Today
Title: Childhood Trauma in Schizophrenia: Current Findings and Research Perspectives
Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6448042/
Written & Published By: NIH (National Library of Medicine)
Title: The Role of Childhood Trauma in Psychosis and Schizophrenia: A Systematic Review
Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8858420/
Written & Published By: NIH