Can Alcohol Cause Depression Relapse?
Depression is a complex mental health condition that affects millions of people worldwide, often requiring ongoing management and treatment. One factor that can significantly influence depression is alcohol consumption. Research has shown that alcohol can exacerbate depressive symptoms and even trigger a relapse in individuals who have previously recovered from depression.
The impact of alcohol on depression relapse can vary between genders; studies suggest that women may be more susceptible to alcohol-induced depression due to biological and hormonal differences, while men might experience more severe depressive episodes as a result of heavy drinking.
Understanding the relationship between alcohol and depression is crucial for both prevention and effective treatment strategies.
Understanding Depression Relapse
Depression relapse refers to the return of depressive symptoms after a period of improvement or remission. It is a common challenge for individuals recovering from depression, with the risk of relapse being higher in those who have experienced multiple episodes.
Various factors can contribute to a relapse, including stress, lack of social support, and inadequate treatment adherence. Recognizing the early signs of a relapse, such as persistent sadness, loss of interest in activities, and changes in sleep or appetite, is crucial for timely intervention.
Effective management strategies often include a combination of medication, therapy, lifestyle changes, and ongoing support. By understanding the dynamics of depression relapse, individuals and healthcare providers can better anticipate and address the triggers, enhancing long-term recovery and quality of life.
Alcohol and Depression: What’s the Link
Alcohol and depression are closely linked, creating a vicious cycle that can be difficult to break. Alcohol is a depressant that affects the central nervous system, altering brain chemistry and exacerbating depressive symptoms. For individuals recovering from depression, alcohol consumption can hinder progress and increase the likelihood of a relapse.
The interplay between alcohol and depression involves both psychological and physiological mechanisms, making it a significant concern for those prone to mental health issues. Understanding this relationship is key to managing both conditions effectively.
- Alcohol is a central nervous system depressant
- Alters brain chemistry, worsening depressive symptoms
- Can hinder recovery from depression
- Increases the likelihood of depression relapse
- Psychological and physiological mechanisms involved
- Significant concern for mental health management
How Does Alcohol Cause Depression Relapse?

Alcohol can cause depression relapse by disrupting the delicate balance of neurotransmitters in the brain, which are crucial for regulating mood. When consumed, alcohol initially produces a temporary feeling of euphoria, but as it is metabolized, it leads to a crash that can intensify feelings of sadness and hopelessness.
Additionally, alcohol impairs judgment and lowers inhibitions, making it harder for individuals to stick to their depression treatment plans. Over time, chronic alcohol use can lead to dependency, further exacerbating depressive symptoms and significantly increasing the risk of a relapse.
The Impact of Alcohol on the Brain
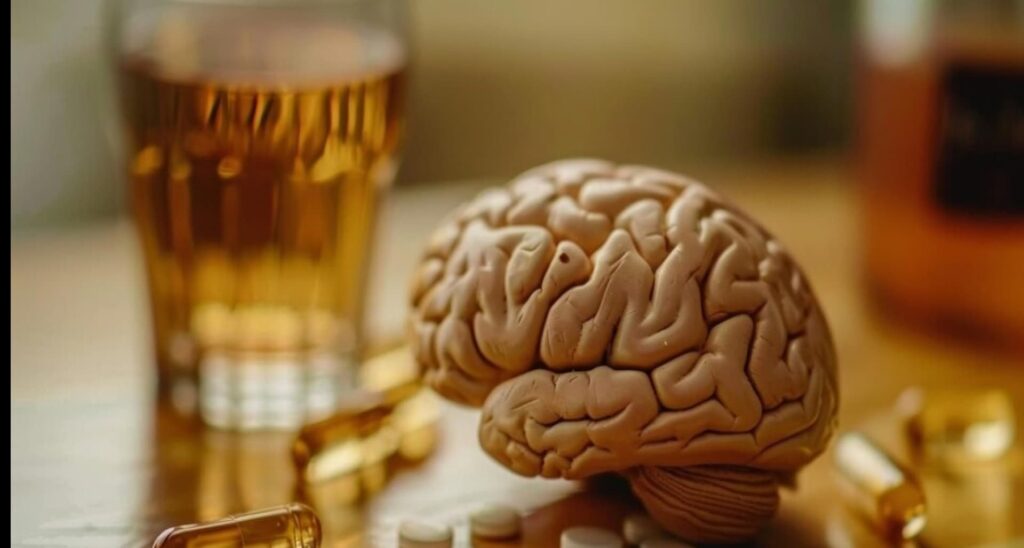
Alcohol has profound effects on the brain, influencing various mental functions and processes. Here are five key effects of alcohol on the mind in more detail:
Impaired Judgment and Decision-Making:
- Alcohol affects the prefrontal cortex, the brain region responsible for rational thinking and decision-making.
- This impairment leads to poor judgment, impulsivity, and an increased likelihood of engaging in risky behaviors such as unsafe driving or unprotected sex.
- As alcohol lowers inhibitions, individuals may make choices they would typically avoid when sober, potentially resulting in harmful consequences.
Memory Disruption:
- Alcohol disrupts the functioning of the hippocampus, which plays a crucial role in forming and retrieving memories.
- Short-term memory loss is common, making it difficult for individuals to remember recent events or conversations.
- In severe cases, chronic alcohol use can lead to more significant memory problems, including blackouts and long-term cognitive impairments.
Mood Alterations:
- Alcohol impacts neurotransmitters such as serotonin and dopamine, which are essential for regulating mood and emotions.
- Initially, alcohol may create a temporary sense of euphoria or relaxation, but as its effects wear off, it can lead to increased feelings of anxiety, sadness, and irritability.
- Over time, these mood swings can contribute to the development or worsening of mental health conditions, including depression and anxiety disorders.
Reduced Cognitive Function:
- Alcohol slows down cognitive processes, affecting the brain’s ability to process information efficiently.
- This reduction in cognitive function manifests as decreased concentration, attention, and problem-solving abilities.
- Tasks that require clear thinking and quick decision-making become challenging, and overall mental performance is diminished.
Dependency and Addiction:
- Prolonged alcohol use alters brain chemistry, particularly affecting the reward system that governs pleasure and reinforcement.
- These changes can lead to physical dependence, where the brain and body require alcohol to function normally.
- Addiction develops as individuals crave alcohol and prioritize its consumption over other aspects of their lives, making it difficult to quit without professional help.
Alcohol’s Physical Effect that Can Trigger Relapse
Alcohol’s physical effects can serve as potent triggers for relapse in individuals recovering from depression. When alcohol is consumed, it affects various bodily systems, intensifying cravings and undermining recovery efforts. Physiologically, alcohol disrupts neurotransmitter activity in the brain, leading to changes in mood and cognitive function.
Additionally, it can impair liver function and weaken the body’s immune system, exacerbating any existing health issues. These physical consequences not only contribute to the cycle of addiction but also heighten feelings of hopelessness and despair, which are common triggers for depressive episodes.
Challenges in Treating Both Conditions Simultaneously
Treating both depression and alcohol use disorder simultaneously presents unique challenges due to the intricate interplay between these conditions. Recognizing warning signs is essential for effective management and prevention of relapse.
Identifying triggers for alcohol consumption in individuals with depression is crucial, as certain situations or emotions can heighten the urge to drink. Strategies for recognizing and managing triggers include cognitive-behavioral techniques, mindfulness practices, and building a strong support network.
Additionally, monitoring mental health is vital, emphasizing the importance of regular check-ins with healthcare professionals. Resources and support systems, such as therapy, support groups, and helplines, are available to assist individuals in monitoring their mental health and accessing necessary interventions.
By proactively addressing warning signs and implementing appropriate strategies, individuals can enhance their chances of successfully managing both depression and alcohol use disorder concurrently.
Prevention and Treatment Strategies
Prevention and treatment strategies are essential for managing both depression and alcohol use disorder effectively. By implementing proactive measures and seeking appropriate interventions, individuals can reduce the risk of relapse and improve their overall well-being.
Dual Diagnosis Treatment Programs
Dual-diagnosis treatment programs address both depression and alcohol use disorder concurrently, providing comprehensive care tailored to individual needs. These programs typically integrate various therapeutic approaches, including medication management, psychotherapy, and support groups, to address the complex interplay between these conditions.
Cognitive-behavioral therapy (CBT)
CBT is a highly effective therapeutic approach for treating both depression and alcohol use disorder. By identifying and challenging negative thought patterns and behaviors, individuals learn healthier coping mechanisms and develop skills to manage cravings, prevent relapse, and improve mood and overall well-being.
Medication Management
Medications may be prescribed to alleviate symptoms of depression and reduce cravings for alcohol. Antidepressants, such as SSRIs or SNRIs, can help stabilize mood and alleviate depressive symptoms, while medications like naltrexone or acamprosate can reduce cravings and support sobriety in individuals with alcohol use disorder.
Lifestyle Changes
Making lifestyle changes, such as adopting a healthy diet, engaging in regular exercise, and practicing stress-reduction techniques like mindfulness or yoga, can significantly impact mental health and recovery outcomes. These holistic approaches promote overall well-being and provide valuable support in managing both depression and alcohol use disorder.
Support Groups and Peer Support
Joining support groups, such as Alcoholics Anonymous (AA) or Depression and Bipolar Support Alliance (DBSA), provides individuals with opportunities to connect with others facing similar challenges, share experiences, and receive encouragement and guidance from peers. Peer support can be a valuable source of motivation and accountability in maintaining sobriety and managing depressive symptoms.
Relapse Prevention Planning
Developing a relapse prevention plan with the help of healthcare professionals is crucial for long-term recovery. This plan outlines triggers, warning signs, coping strategies, and emergency contacts, empowering individuals to anticipate and effectively manage potential setbacks in their journey toward wellness.
What Organ Does Alcohol Affect the Most?
The organ most profoundly affected by alcohol consumption is the liver. As the body’s primary detoxification organ, the liver bears the brunt of alcohol metabolism. When alcohol is consumed, it is broken down in the liver by enzymes, producing harmful byproducts such as acetaldehyde, which can damage liver cells and impair function over time.
Chronic alcohol use can lead to various liver conditions, including fatty liver disease, alcoholic hepatitis, and cirrhosis, which can have serious health implications and even be life-threatening.
Additionally, the liver plays a crucial role in metabolizing medications and filtering toxins from the bloodstream, so alcohol-induced liver damage can impact overall health and well-being.
The Bottom Line
While alcohol may initially provide temporary relief or relaxation, its long-term effects can exacerbate depressive symptoms and increase the risk of relapse in individuals recovering from depression. Understanding the impact of alcohol on mental health, including its effects on brain chemistry, mood regulation, and overall well-being, is essential for prevention and effective treatment strategies.
By recognizing warning signs, seeking appropriate interventions, and implementing healthy coping mechanisms, individuals can mitigate the risk of alcohol-induced depression relapse and work towards long-term recovery and wellness.